Insider Insight into VBA Claim Processing
Congratulations on obtaining one of Veterans Benefits Administration (VBA) golden tickets. You have earned a guided tour by me, the one and only, Richard Strange! You will receive unprecedented access into the VBA's processes from an insider's perspective.
Hopefully you are wearing clothes you do not mind getting dirty!
We do respectfully remind you to please observe our rules and sign our release, before we enter the building.
Rules:
NO eating
NO drinking
NO feeding VBA staff
NO flash photography
NO disparaging the tour
Not responsible for lost or stolen items, death or dismemberment, or soiled clothes. Known in the state of California to cause cancer. No purchase necessary, void where prohibited.Ground Floor (Public Contact Team (PCT) and Intake Processing Center (IPC))
Come, come! Here at the front desk we have the Public Contact Team (PCT). These bright eyed and bushy tailed souls are tasked with:
Discuss with people the eligibility requirements for the benefit(s) they are seeking;
Assisting in the completion of application(s)/form(s) for benefits;
Advising on any additional information/evidence the Veteran Service Center (VSC) requires to process the claim or adjust the award;
Date-stamp any documentation received;
Answer questions submitted via AskVA;
Update the VBA record based on new/additional information provided (such as an updated mailing address, direct deposit information, and/or corrections in date(s) of birth and Social Security number(s), etc.); and
Route all documentation that requires action (other than updating the corporate record) to the VSC’s IPC or to the scanning contractor.
Around the corner we have the Intake Processing Center (IPC). These people hold the formal title of Claim Assistants (CAs) they are tasked with:
Establishing new records and claims folders when warranted;
Managing outgoing paper mail; and
Processing and controlling mail received in the Centralized Mail (CM) portal.
This is where Stage 1: Claim Received can take place. While claims are generally established by machines; CAs can establish claims/appeals.
Now follow me to the elevator.
Basement Floor (Veterans Service Representative (VSR))
Please be mindful of the piles of empty Everclear bottles on the ground as we continue down the halls everyone! Ah, here is a VSR sitting at their desk. Let's ask them what they do here.
Veterans Service Representative (VSRs) are commonly tasked with:
Ensuring claim/appeal paperwork have been completed properly;
Updating the VBA record based on new/additional information;
Requesting various records including but not limited to: military, VA, and private records;
Sending requests for information/clarification;
Reviewing evidence;
Ordering examinations; and
Sending notices.
For a full list of responsibilities click HERE.
The overarching purpose of a VSR is to gather relevant evidence so that Rating has everything it needs to make their decisions.
VSRs use the Veterans Benefit Mangagement System (VBMS) to do their jobs. This application allows them to work claims/appeals by giving access to Veteran's Claim files.
Once assigned to a VSR for the first time, the claim enters Stage 2: Initial Review.
Starting Work
When a VSR starts their day they look at their claim queue. This queue contains their new piles of claims for the day (given to them in the morning by the National Work Queue (NWQ)) as well as the piles of claims they may not have gotten to from the previous day(s). The goal is to process things within 5 business days of work being assigned.
As to how a VSR picks the order to work things, the VSR should work older claims and those with Priority flags first. However in practice, some VSRs will pick the 'easier' (smaller claims) to work first.
Most VSRs prefer getting a fresh claim that has not been worked by another VSR. By having a fresh claim, you have a clean slate you and do not have to investigate what the last person(s) did/did not do and what still needs to be done.
IMPORTANT NOTE:
The way VBA assigns quality errors is based upon who was the last person to work the claim. Meaning, even if someone should have done something months ago - if you do not fix it YOU are the one who eats the error; if you do not take the correct steps to fix the error(s). Furthermore, the person who made the initial error(s) gets away free - unless they happen to be audited immediately afterwards and caught first. This fosters a mentality of trust no one (for good VSRs) and checking EVERYTHING, EVERY TIME. For bad VSRs this provides a means to do a poor quality work and by-in-large, not be held accountable. Which of course leads to claims being delayed for months and potentially denied in error due to bad/missed development.
Going into a claim file the first checks that should be done are 'system checks' which boils down to ensuring administrative stuff is in order and correct:
Vet information: Name, date of birth, SSN, address, etc.
Periods of service and character of discharge
Power of Attorney of record
System checks complete, time to check the paperwork:
Completeness of Paperwork
Proper signature(s)?
Check claimed condition(s)
Was anything previously denied?
Does the Veteran need to be contacted to get clarification?
Did Veteran mention other disabilities in the description of the claimed condition? If so, it may be appropriate for VA to consider those issues as claimed as well.
Date paperwork was received by the VBA
Used to help establish 'date of claim'. Which is mainly for internal VBA claim tracking purposes.
Review evidence submitted with claim
Did Vet mention treatment at a private medical facility? Did they submit those records? If not, VA needs to send a release to attempt to get those records.
Did Vet mention other disabilities in the description of the claimed condition? If so, it may be appropriate for VA to consider those issues as claimed as well.
After reviewing the paperwork and evidence received, it is time to check the 'claim tab'.
Claim Tab
The claim tab is infamously what Veterans see when they check the status of their claim - in terms of claimed conditions and if it is primary or secondary condition. Now-a-days it is common for most claims to be automatically generated in VBMS. Sometimes... the machine really struggles. This results in claimed issues showing up with weird misspellings or just nonsense.
It is the responsibility of the VSR to make sure the claimed issues are properly accounted for in the claim tab. Which can get really tedious if there are a ton of conditions.
Reviewing Records
If the records are already in the file then a VSR needs to painstakingly look over EVERY page to ensure any and all in-service complaints are noted. This can be a quick process if someone never went to sick call or it can take several days if someone served for decades and has tens of thousands of pages to review with plenty of bad doctor's handwriting and microfiche that is out of focus and looks like someone threw it into a drier with a bunch of sharpies and knifes!
Additionally medical records created after separation are reviewed, but this review is purely to note treatments/history/diagnoses.
IMPORTANT NOTES:
Your claim file is a PERMANENT record. Meaning any and ALL evidence obtained by the VA no matter how many years ago is apart of your record. For dusty Vets that had physical files those have been digitized and made apart of your virtual claim file. Meaning do NOT resubmit evidence! This makes reviewing records more difficult and increases the likelihood that something will be overlooked.
There is no separation of evidence submitted for any claims/appeals. Everything is dumped into your claim file. While sure, a VSR can mark files as being associated with a claim - it is not done with any frequency since a VSR should be reviewing the entire file for evidence anyway.
Medical Examinations/Opinions
If the records review finds that exams are Warranted they will be ordered. As far as medical opinions go, if a Veteran claims something as secondary but the review shows in-service complaints of something; the VSR needs to order a direct opinion in addition to the secondary opinion. However, if a condition is Presumptive AND the Veteran has appropriate service then the VSR should NOT order an opinion for the condition.
In the case of claims made while on Active Duty or within a year of separation, we order a General Medical Examination (basically looks over everything you claimed and anything you bring up to the examiner). We do not order medical opinions - unless we notice a condition is preexisting on the entrance physical, in which case we will ask a rater to make an Aggravation opinion request if appropriate.
Ready to Return
When everything that needs to be ordered/requested is done and the tracked items are created then the claim will generally automatically become 'ready to return', meaning that at the end of the day the claim will return back to the NWQ to come back down after the the suspense date has passed.
The claim will now enter Stage 3: Evidence Gathering.
Claim Returns
When a claim comes back down from the NWQ, it enters Stage 4: Evidence Review; know it can come down to the same Regional Office or to a random one.
*Finishes bottle of Everclear*
Now this is where the fun really kicks off.
In a perfect world a VSR who is getting a claim back from the NWQ would just need to check the tracked item tab and check the claim file to see that the requested things have come in. If something came in great! Mark it as received and if something has not come in then extend the suspense date another 30 days (if appropriate)...
However, it is best policy just to treat things as if another VSR has not touched the claim. This is because again, trust no one! While sure, this takes a lot more time than just slapping the claim on the ass and marking things good to go or ready to return... errors abound. The amount of times appropriate exams/opinions/records are not requested - that and other issues, are just staggering.
If the claim is still missing appropriate evidence the claim is returned to Stage 3: Evidence Gathering.
Ready for Decision
Once the VSR gets a claim and development has been completed (so that at least 1 issue can be decided) then the claim is marked as Ready for Decision (RFD) by the VSR.
The claim now enters Stage 5: Rating.
NOTE:
If there is at least 1 issue that can be rated the entire claim should be sent to rating immediately, even if development may not have been completed on every issue. This of course helps to speed a claim along and not get hung up waiting potentially months for one thing! Unfortunately, this is rarely done.
If any VSR wants to fight me on This or This; accept the calendar invite and meet me in the Rumble Room on the 13th floor!
Richard Strange: Thanks for your time! Come along everyone, time to go deeper and enter the rating dungeon!
Unknown Depth (Rating Veterans Service Representative (RVSR))
And here is were we keep the raters!
*As the elevator doors open, a wall of humidity and the sounds of groans and cries flood in*
We have a rater you can talk to located in the Last cell, we pulled out some chairs for you all. I won't be joining you, but I will be watching.
*Elevator doors close with a thud, as the group walks down the dank hallway*
Rating Veterans Service Representative (RVSRs) are tasked with:
Ensuring claim/appeal paperwork have been completed properly;
Ensuring all Duty to Assist obligations have been satisfied;
Reviewing evidence;
Ordering examinations;
Properly assigning evaluations and effective dates.
For a full list of responsibilities click HERE.
Just like VSRs, raters are assigned claims via the NWQ. Again, the goal is to process all assigned claims within 5 business days.
It is important to know that the NWQ is far beyond mere mortal understanding. Claims raters get could have been marked RFD the day prior or more than 3 months ago! The only thing that stands to reason is that claims marked as Priority DO seem to get to rating faster more often than not.
RATER NOTES:
In the case of claims of Lou Gehrig's disease (ALS), which have an exceptionally high priority, those will receive a partial decision the same day VA gets the claim (assuming appropriate service can be verified and a diagnosis is of record). So if appropriate, service-connection at the 100% rate will be given in addition to various ancillary benefits; the rater will defer for a medical examination to determine the current severity of ALS residual condition(s). This usually results in grants of upper levels of Special Monthly Compensation (SMC) depending how progressed the condition is.
This is because the disease can progress VERY QUICKLY and delaying even a day can result in the Veteran passing away before a decision is made.
Trust No One - Reviewing Evidence
A good rater should trust no one and have faith only in the evidence of record!
An ironic thing about being a good rater is that good raters will spend most of their time... not actually rating. No, I do not mean they are farting around watching Netflix. I mean they are investing the time to make sure the claim has been properly developed and that the VAs duty to assist has been completed.
The VAST majority of claims that come before a rater are not fully ready for decision. Now to be fair to VSR's, this is not always their fault. Sometimes medical examiners overlook evidence, mess up a DBQ, or provide an insufficient medical opinion. But other times, rating will get claims with exams not ordered or medical records not obtained! At the absolute worst, sometimes claims will make it to rating after nearly a year and the claim paperwork will be invalid (paperwork not being signed)!
For every claimed condition, the rater should always review the evidence of record! While it seems obvious, we know this isn't always being done unfortunately... This review will fairly often result in finding that required exams/opinions were not ordered by the VSR.
Medical Opinions
Raters are not medical professionals and CANNOT provide medical opinions, which is why VA requests them. Meaning, if you get a bum examiner who wrote an unfavorable medical opinion the Veteran is in a bad spot... HOWEVER, if a medical opinion's rationale is trash the rater CAN kick it back and either request clarification (umm hey you said medical records were silent... but pages x, xx, xxx, xxx, mentioned issues with the right knee while Veteran was in-service, can you please review and update your opinion as appropriate?) or in the cases of presumptive conditions simply override the unfavorable opinion. For Presumptive conditions, it takes an Extremely detailed medical opinion to overturn a presumptive condition. Yes, VSRs should NOT be requesting medical opinions for presumptive conditions... but it happens.
If the Veteran claimed a condition as being secondary to something and the examiner provided an unfavorable medical opinion BUT there is evidence in the military medical records that the condition may have begun in service, the VA has a duty to assist to request a direct opinion.
Examiner Being a Bro
If the Veteran claimed a condition is directly due to their military service but the examiner states it is due to a service-connected condition instead - the rater CAN and SHOULD grant the condition on a secondary basis! While this situation is uncommon (the examiner volunteering medical opinions), it does happen.
If the examiner does a bunch of extra DBQs for you. The rater may or may not be able to grant you service-connection if appropriate. This is because unless these conditions are considered 'within the scope' of your claim, the rater is NOT authorized to raise the issues.
The matter of not being able to raise obviously service-connected conditions exists even outside of the medical examiner giving a helping hand. If the evidence of record shows a Veteran is entitled to presumptive service-connection for something - the rater CANNOT just grant service-connection in most cases!
What the rater can do is 'invite' the Veteran to file a claim for those conditions. While invitations are not always appropriately done by raters - for the most part if you see text in your decision letter that states 'you may be entitled to service-connection for X', it would be a great idea to file a claim.
NOTES:
Scope of claim can be described as: something the VA can reasonably consider to be meant to be filed for as well.
Common examples include:
Residual Scars from surgery of a service-connected condition;
Claimed Hearing loss but the exam notes Tinnitus;
Claimed Sinusitis and exam notes Allergic rhinitis (or vice-versa);
Claimed Spine condition and the exam notes Nerve issues; and
Claimed Diabetes and the exam notes Complications of diabetes.
IMPORTANT NOTE:
The VA has expressed through Policy that arteriosclerotic complications of Hypertension are NOT considered to be within the scope of a claim! Meaning for the VA to consider, the Veteran needs to file a claim!
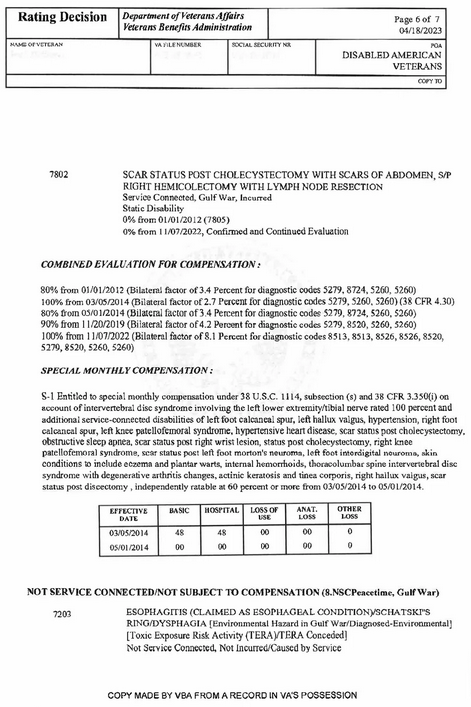
Rating Decision
Now with all that time spent checking the evidence and seeing what still needs to be done, raters can now start rating.
Again, a bad rater would start here - while sure they will save a lot of time, they are doing a great disservice to Veterans. It just makes too much sense to spend those extra hour(s) if necessary to prevent denying a Veteran and having them wait months/years in appeals over something very stupid.
Before we get deeper into things I will disspell a rumor:
IT IS FAR EASIER FOR A RATER TO GRANT SOMETHING THAN DENY!
The VA does NOT encourage raters to deny Veterans!
Raters do NOT look for a reason to deny!
I spend the vast majority of my time helping to ensure I can grant as many things as possible! Hell it is not my money!
Raters do not use VBMS (core) to enter decisions, raters use Veterans Benefit Mangagement System - Rating (VBMS-R); which is a sister integrated application to VBMS and R pulls data from the claim from VBMS (core) to make things easier.
When building a decision, the rater needs to input the claimed issues. Thanks to their integration, R will show a list of issues (as they appear in core). However, if a VSR missed a claimed issue then it of course will not show up. So it is again critical for a rater to personally review and check everything and not blindly trust the work of others!
To enter a decision, the rater will grab one of the issues and will either 'manually' enter a decision or select one of the rating calculators (Muscleskeletal - ankle, Hearing, etc).
In general there is no hard set rules when it comes to evaluating medical evidence; meaning raters have a fair bit of freedom when it comes to setting up the scales. Weights on the scale may include but are not limited to:
Education of medical provider to include specialization(s);
Length of practice;
Depth of supporting evidence (how personalized is it - was the Veteran's specific medical records referenced or just hand waving and a mention of a study); and
Causation vs. correlation.
While yes, a rater is not a medical professional - a rater CAN weigh medical evidence. In the event the rater cannot make heads or tails of the evidence then tie goes to the Veteran's favor. This does NOT mean that if there is a one negative opinion and one favorable one than the rater needs to grant!
Granting
If after reviewing everything and it is all good, then happy days! The rater selects the appropriate rating calculator and plugs in the severity of the condition. These calculators match up exactly to the Rating schedule.
IMPORTANT NOTES:
These rating calculators MUST be used by a rater. There is no overriding what is spits out in terms of an evaluation, with the only exception being Mental health. The mental health calculator generally spits out 3 different evaluations: One suggested evaluation and two overrides - the overrides being 1 higher or 1 lower than the suggested.
Most evaluation criteria are black and white. Though, for things like mild, moderate, etc. severity, the rater for the most part has the freedom to weigh evidence and make a determination.
Do know that for the most part medical evidence outside of DBQs are not detailed for rating purposes and is not useful. However, a rater MUST look over everything to properly evaluate a condition. If there is conflicting evidence then the rater needs to evaluate the evidence and determine how to proceed:
Do we need to contact the examiner for clarification?
Does the evidence indicate the severity of the condition changed over time?
If so, then a Staged evaluation would be appropriate.
Service-Connection, Effective Date, Bilateral Factor
After an evaluation is determined, the rater will input if service-connection for the condition is direct, secondary, etc. as well as what period of service the injury was due to (purely administrative bean counting by big VA).
Conditions that have a Bilateral factor consideration have a drop-down which the rater will select (left/right upper/lower) as appropriate.
For Effective dates, the system does have a 'helper' which spits out a suggested effective date. The system is only as good as the data in VBMS, so if things are incorrectly input into that system the helper can spit out incorrect effective dates. Furthermore, the helper... is NOT too smart, so in cases which involve anything more than basic situations - it WILL give incorrect dates! So a rater needs to pay attention to all the evidence and specifics of the claim/condition they are adjudicating!
Narrative
Once that data is all decided, it is time for the narrative of the decision for the issue.
Outside of explaining overrides, everything is auto-generated by VBMS-R thanks to the rating calculator.
Denying
If VA has exhausted its duty to assist and there are no routes to service-connection the rater can go down, the claim must be denied.
Most of the time it is not a matter of the rater not believing a Veteran's claim, just the evidence of record is not strong enough to support a claim.
While VBMS-R does offer canned language for denials (most of it being required) the rater should explain in detail why a condition is being denied. Good raters leave a roadmap behind in their decision to give a Veteran a clear direction as far as what is needed to win an appeal. But all too often raters will deny with little to no explanation.
Favorable findings are a required part of a denial - if they exist. Favorable findings boil down to the claim having 1 or more of the 3 Elements needed for the VA to grant service-connection.
Deferrals
Deferrals are not inherently good or bad things, they just mean the rater could not make a decision one way or the other due to missing evidence.
Depending how bad things turned out during the development process, it can result in a few deferrals to the an entire claim being kicked back!
When a rater defers something, they must identify ALL issues that need to be fixed in the claim. This process can be very taxing when there has been large amounts of bad/missed development. So while a rater's job is not technically to do claim development, a good rater needs to be experienced in claim development to know when errors have occurred. Unfortunately, people hired off the street as a rater who did not start as a VSR do not start with great insight on claim development, as rater training... maybe touches the littlest of pinkies into the development pool. In a perfect world that would not be too big of set-back, but with so many new VSRs it become a major issue.
Raters must input a deferral in both VBMS and VBMS-R. The deferral in VBMS are detailed instructions telling the VSR what they missed/need to do; while the deferral in VBMS-R is commonly a single sentence 'claimed condition is deferred for: record development'.
Often enough, due to the amount of time it takes to create deferrals: Most raters find it best just to complete/start the missed development issues themselves - at least in terms of ordering/requesting reworks of examinations (clarification/insufficiency). But for sending requests for records or other communications, most raters will just have the VSR do them.
Making a partial deferral (with at least 1 decision) or a full deferral (no decisions made) will result in the claim reverting back to the earlier claim status stages. It of course will also add potentially months to the length of a claim/appeal.
Return of the Prodigal Claim
Raters may or may not get the claim back that they previously deferred.
If a rater gets their own deferral back there is still a chance that:
Examiner did not properly complete the rework properly;
Rater overlooked something and finds there is still something else that needs to be done (additional deferrals to make); and/or
VSR did not correctly complete/start all the noted deferrals.
Raters who get deferred claims from other raters may additionally find that the deferred reasons were:
Over-development: Not relevant to a claim decision (requesting personnel records when Veteran does not have a current medical diagnosis);
Issue raised and deferred in error (sometimes raters will erroneously raise an un/claimed issue improperly - be it due to improper form usage or the issue is outside the scope of the claim);
Failure to make a partial decision: If the rater can grant service-connection but there is an issue determining the correct evaluation. The rater should grant and defer only the final evaluation part - that way the Veteran can get some benefits going at least, sooner than later; and/or
Could have been a phone call/email.
While it is exceptionally rare, raters can and should directly contact Veterans to get clarification on simple things instead of doing a deferral.
Overall, these issues can add even more MONTHS in delays! Worse still, some examiners are SUPER dense and it may take multiple times going back and forth to get them to do their jobs properly.
Basic Error Check
When the rater has finished their decision, the system will do a scan to identify errors. Common errors the system identifies are:
Veteran has a combined evaluation of 100% with no future evaluations but DEA has not been awarded;
Statutory requirements for SMC S have been meet but not awarded;
Common Pyramiding issues; and
Entitlement to 38 CFR 3.324 not addressed.
Draft Decision
After passing the basic error check the rater will generate a draft decision. This is to help make sure there are no errors in a decision. Obviously, this is not fool proof, but it does cut down on mistakes.
There are two parts to a draft decision:
Rating narrative; and
Rating codesheet.
Rating Narrative
This is the rating decision you see. Raters should be proofreading everything to make sure it makes sense and to double check that a claimed issue was not overlooked. Mistakes such as contradictions regarding effective dates or evaluations should not exist!
2. Rating Codesheet
The codesheet is the true backbone 'master record', which contains previous important stuff like grants, denials, current deferrals, current/past combined evaluations, etc. It is also what matters in terms of how Veterans are paid, meaning if the codesheet is wrong but the narrative is 'right', then things are not right! If a narrative is wrong but the codesheet is right, then things will be right for the Veteran - at least administratively.
So of course a rater needs to be sure their narrative matches up with their codesheet!
With experience, raters can also quickly scan a codesheet and identify previously committed Clear and unmistakable errors (CUE). At the very least, things on a codesheet that should demand a closer inspection by the rater to find out if a CUE does exist.
NOTES:
If a rater misses a CUE done by a past rater and the file is pulled for an audit. The last rater who touched the file will be tasked to correct the CUE. Furthermore, missing the CUE will not count against that rater.
If a CUE is found by the rater, then the discovering rater is the one who has to declare the CUE and fix the issue. If the error goes against the Veteran, due process may be required - if the error results in over-payment or severance.
There is no punishment for the rater who made the CUE.
Finalizing
Once everything looks good to go, the rater will finalize their deferral(s) and rating decision. This will plop a copy of both the rating narrative and codesheet into VBMS.
The claim is then sent to be promulgated and authorized and the claim stage progresses to Stage 6: Preparing Decision Letter.
Rater to group: Pist...Please send help, I haven't seen my family in months... Richard Strange: *Plays flute* We can't be having any of that now! Rater: Where did you come from! Richard Strange: But... having them come in to work claims does sound like a good idea! Zoompa, doompa (ZD): Zoompa, doompa, loompa-dee-do Rater: Please no! ZD: I've got a perfect puzzle for you ZD: Zompa, doompa loompety-dee ZD: If you are wise, you'll listen to me ZD: What do you get when you think about escape ZD: Dreaming that you will get out without a scrape ZD: Where are you at? Getting terribly fat ZD: What do you think will come of that? ZD: I don't like the look of it ZD: Zompa, doompa doompety da ZD: If you're not lonely, you will go far ZD: You will live in happiness too ZD: Like the Zompa Loompa loompety do ZD: Loompety do
7th Floor Promulgation and Authorization
Howdy everyone! Welcome to the 7th floor! Home of the Post and Senior VSRs!
We have been expecting you.
Oh! They probably never explained did they? So, the basement dwelling VSRs are known as "Pre" VSRs, since they do claim development. We Post VSRs handing things after the rater!
Our primary tasks include:
Reviewing the rating decision/codesheet for errors;
Reviewing claim/appeal paperwork for errors;
Setting Withholding of money;
Sending out notifications;
Generate award/decision letter; and
Authorizing.
Last Saviors
We are the final safety net to catch any errors. However, our ability to catch errors is fairly limited outside of fairly obvious ones (effective date does not seem reasonable, missed claimed issues, contradictions in the rating decision narrative/codesheet, etc.); as we are not ourselves dirty raters.
If we find an error we will defer the rating back to the rater for correction. Though, sometimes to help speed things up we will reach out directly to a rater to ask them to do a quick fix instead of deferring. However, some errors are so bad that nothing from a rating decision can be saved! These errors usually take the form of there being a duty to assist error and the rater denied things or significant paperwork issues.
The perhaps biggest day killer for raters is when we find that the VSR failed to send a required 5103 notice and the rater also misses it. In those cases, if the rater's decision has a denial in it - they in most cases will have to redo/undo their decision and defer the claim to allow for the notice to be sent and wait out the 30 day period of the notice.
Award
No errors means we can process the rating decision and setup any withholding of pays (if appropriate) and generate the award/decision letter. If the rater requested that we invite any claims, we will include that invitation in the decision letter. Oh, and if claimed Dependent(s) AND the rating decision just made you at least 30% combined then we will add them now as well! Otherwise if you were already previously 30% combined... then... well the Benefits Eligibility Support Team (BEST) people handle dependent claims... and No, no, no, we don't talk about BEST!
With all that done, we then send things to the final link in the chain.
At this point the claim enters Stage 7: Preparation for Decision Notification (Final Review).
Wrapping Up
Okay... so there is a final final check of things done by a Senior Veterans Service Representative (SVSR). The title is a bit misleading as they are NOT senior raters (and are generally not former raters), but they are experienced in processing rating decisions.
If an SVSR finds an error done by the Post VSR, the claim will go back to the Post VSR. If the SVSR finds an error by the rater, the claim will go back to the rater.
But if all is good things will be authorized and get all dolled up! With the rating decision being sent out to the Veteran upon the backs of the fastest imported French racing snails to the Veteran. The snails typically reach the Veteran within 2 weeks... Though, if you are in a rush, you can view your decision letters online HERE.
The claim is now complete (unless there are any deferrals) and enters Stage 8: Complete (Claim Decided).
Conclusion
That concludes your tour, don't forget to check out the gift shop!
Frequently Asked Questions
-
Well... yes/no. Only if the rater is assigned a claim/appeal and the rater notices that the 'sister' claim/appeal the Veteran has, has at least 1 issue that is ready to be rated, the rater can ask their supervisor to assign the sister claim/appeal to themselves.
This picking up CAN be done even if the claim/appeal was not previously marked as ready for decision.
Do know that a rater CANNOT rate sister claims/appeals outside of the rater's jurisdiction. This includes but is not limited to certain special issues such Camp Lejeune, Military Sexual Trauma (MST), Higher level reviews, etc.
Raters also are prohibited from rating claims and appeals at the same time IF the Veteran has a private attorney representing them. This is due to the VA system being really dumb when it comes to determining what the attorney is owed if the rater rates them together.
-
Claims can be worked during most holidays/weekends. Though sometimes overtime is not authorized or there is some maintenance being done which prevents claims from being worked.
-
A well seasoned VSR can process around 15 claims over an 8 hour work day.
-
A well seasoned rater can rate around 3-4 claims over an 8 hour work day.
-
It can take as little as under 30 minutes to over 15 hours to rate a single claim; depending on the various degrees of complexities. But most claims can be rated in around 2 hours.
-
Most of the time an attorney adds little to nothing in terms of helping an appeal. A lot of attorneys will use boilerplate statements which generally do nothing but make a Veteran think they are in good hands.